|

download Chinese version 
Disturbances of Digestive and Bowel Functions – Answers to Your Questions
Functional disorders of the digestive and bowel systems are the commonest causes of symptoms such as abdominal pain, bloating, indigestion, belching, flatulence, constipation, diarrhoea, incomplete bowel movements and changes in stool consistency.
Irritable Bowel Syndrome
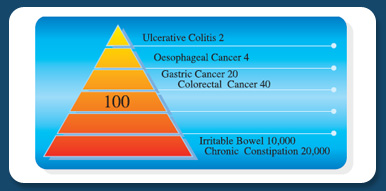
It is estimated that close to a million people in Singapore have these symptoms. Patients and doctors usually worry that these symptoms could be due to diseases like infections, gallstones, ulcers or cancers. However, every year the number of people with these functional disorders such as irritable bowel syndrome, chronic constipation and functional dyspepsia outnumber the people with all the cancers of the digestive system by 500 times.
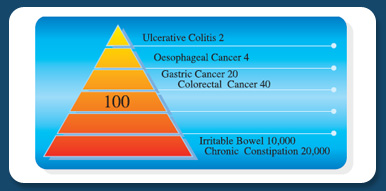
Incidense of Chronic GI Diseases (per 10,000 per year)
Despite the fact that there is no serious disease, these functional disorders frequently impair the quality of life. This need not be the case because when these patients are appropriately managed, in the majority their symptoms will largely disappear. In order to achieve this it is important to provide accurate and sound scientific information.
How can I confirm whether I have IBS?
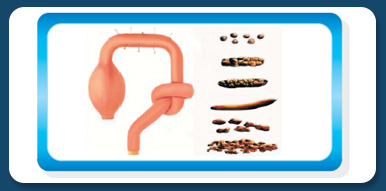
IBS is not a condition that is diagnosed simply by doing blood or stool tests, x-rays, ultrasound scan or even endoscopy. On the other hand, IBS can be diagnosed by listening carefully to the patient’s history. First of all there must be symptoms pointing to the bowel as the likely source of origin. These include a disturbance in the bowel habit, and a variation in the stool frequency and or consistency with the abdominal pain or discomfort, and whether the pain is relieved with passing stool.
Symptoms of IBS
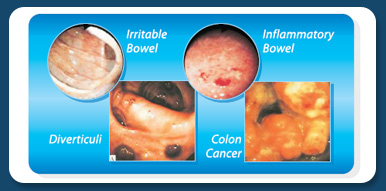
However, these only tell us that something is irritating the bowel – the cause of this disturbance can range from irritable bowel to infection to even cancer. While colonoscopy and barium enema are not tests to diagnose IBS, they serve to exclude the other causes. It is also important to remember that just because a person has IBS, does not mean that he cannot also have some other disease like ulcers and cancers.
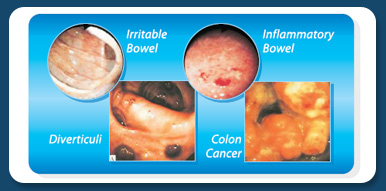
Chronic Bowel Diseases
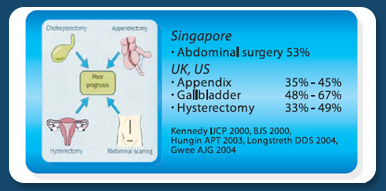
Logistically it would be near impossible to send all patients with IBS for tests (there is an estimated close to half a million sufferers in Singapore), and many patients themselves are not willing to go for tests. Therefore the doctor will try to help the patient by taking certain factors into consideration in deciding whether further tests are required. Important considerations are whether the symptoms are longstanding or recent, and whether they fluctuate or are progressive. It is also important to know whether there are sinister symptoms such as weight loss and blood in the stools, or whether there are other functional type symptoms such as headaches, tiredness and shortness of breath. Life would be much easier for doctors if all patients could go for the relevant tests. However, I would caution that it is important to go for relevant tests. For example, if irritable bowel is suspected, undergoing an ultrasound scan to detect gallstones is not only unnecessary, but often produces unnecessary anxiety, leading to surgery to remove the gallbladder, an operation that could make the IBS worse. However, there is evidence that for many IBS patients, undergoing a carefully justified set of tests can often in itself result in an enormous improvement in their symptoms.
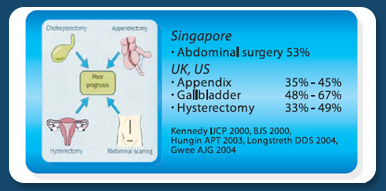
Excess Surgery in IBS Patients
Is there effective cure for IBS?
There is clear evidence that the disturbances in IBS can be largely resolved. To achieve this, both the doctor and patient have first to be confident and comfortable with the diagnosis. The doctor will have to ask detailed and probing questions, sometimes accompanied by a carefully selected set of tests, to get an understanding of the patient’s problem. It is not enough just to know that the patient has IBS. It is important also to define, and determine the numerous factors that contribute to, the type of disturbed functions. Next the patient has to be helped to develop a clear understanding of the condition, paying particular attention to the role of lifestyle and psychological factors. Some patients will also benefit from treatment with medications, but these have to be carefully selected. Last but not least, unnecessary surgery should be avoided.
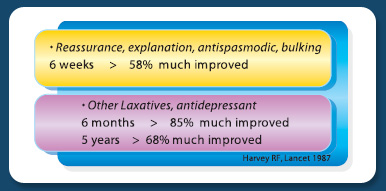
Studies from the UK reported that after a period of treatment with a combination of 2 to 3 simple medications for 6 weeks to 6 months, upto 85% were free of symptoms. Studies from the US emphasized the importance of doctors spending time to listen, and to talk to their patients. In contrast, in one study from the US the majority of women with IBS who underwent laparoscopy or hysterectomy did not improve after their surgery, while studies from Europe reported that patients who underwent surgery to remove the gallbladder thinking that this would take away their IBS symptoms were often disappointed.
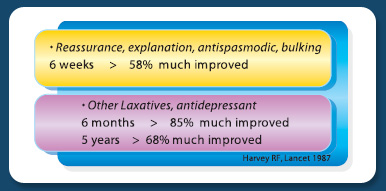
Outcome of Treatment for IBS, a 5-year prospective study
What is the difference between IBS and lactose intolerance?
The term lactose intolerance is often used loosely to mean the same thing as lactose malabsorption, which means poor or reduced absorption of the natural sugar found in milk which is known as lactose. The majority of people of Asian origin and especially Oriental races, are poor at absorbing lactose because of a low level of lactase enzymes in their intestines. However, studies have shown that even after drinking the equivalent of lactose found in four glasses of milk, only one-third of people who are lactase deficient will experience symptoms of bloating, cramps, diarrhoea and flatulence. Thus, there are other additional conditions that may have to be present before a person experiences lactose intolerance. These include the rapid movement of food through the intestine, increased sensitivity of the intestine to gas, and an imbalance of bacteria in the bowels. Some of these conditions overlap in people with lactose intolerance and IBS.
Food Intolerance
Is burping part of IBS, and how do I cope with this?
Belching or burping refers to the release of gas from the stomach otherwise known as eructation. The commonest cause is a condition known as functional dyspepsia which is a disorder of contractile and sensory functions, much like irritable bowel syndrome, except that this involves the stomach rather than the bowels. Other causes for frequent belching are stomach ulcers, acid reflux or GERD, and less frequently, stomach cancer. The usual advice is to avoid gas producing foods such as milk and dairy products, artificial sugars and sweeteners, and to take time to chew well and eat slowly to reduce the swallowing of air. If it still bothers you, do consult a doctor to help you to determine the contributory causes. Treatments that may help include medications to improve gastric emptying, to reduce acidity and to reduce the sensitivity of the nerves in the stomach.
Is gastritis a cause of IBS?
The term 'gastritis' means inflammation of the stomach. Causes for gastritis include Helicobacter pylori infection, painkillers including aspirin, alcohol and smoking, but there are many people for whom no cause can be found. Strictly speaking gastritis can only be diagnosed after a sample (biopsy) is taken of the stomach lining, and sent for analysis. Unfortunately, 'gastritis' is often used loosely to refer to any discomfort experienced in the stomach area. Many patients who experience so-called 'gastric-pain' do not in fact have 'gastritis'. There are also people who have true gastritis who do not experience any pain or discomfort. Many times doctors use the term 'gastritis' simply because it is easier to blame symptoms on inflammation of the stomach than to try and explain the very complex irritable bowel syndrome.
NEXT PAGE
|